484
Views & Citations10
Likes & Shares
Abbreviations: CBCT: Cone Beam Computed Tomography; RC: Radicular Cyst; CT: Scan-Computed Tomography Scan; T-PRF: Titanium Prepared Platelet Rich Fibrin
In children, pertaining to the primary dentition, the occurrence of radicular cysts is rare representing only 0.5-3.3% of the total number of cysts and most commonly involving mandibular molars. Cysts with smaller size usually heal following simple endodontic therapy consisting of root canal treatment. Whereas larger sized cysts require additional treatments such as surgical intervention including marsupialization and cyst enucleation. Clinically, untreated, asymptomatic radicular cysts undergo expansion, causing local tissue destruction and deformities within the jaw [1-4].
There are numerous reports showing occurrence of radicular cyst within the oral cavity involving either primary or permanent teeth because of high incidence of pulpal pathology in the oral cavity [1-4]. Sometimes, they also arise from the carious tooth or improperly restored tooth or traumatized teeth or seen even in root canal failure cases. Development of radicular cyst arising from Odontogenic inflammation and extending to the maxillary sinus is a rare phenomenon. Extensive review of dental literature regarding occurrence of radicular cysts in the maxillary sinus revealed few cases indicating the rarity of its nature [3-11]. Therefore, the purpose of this article is to present a case of asymptomatic giant radicular cyst involving the entire left maxillary sinus in an 18-year-old female Indian patient which was diagnosed on Cone-Beam Computed Tomography scan (CBCT).
CASE REPORT
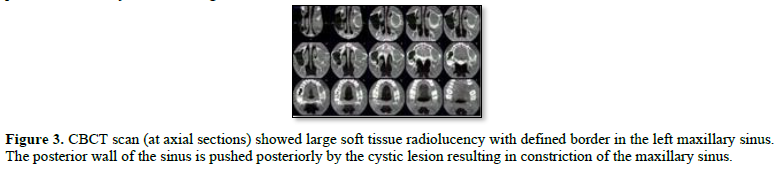
An 18-year-old female patient reported to a private dental clinic wishing to replace her missing tooth in the upper left back tooth region. Patient was moderately built, appeared healthy with no history of any systemic problems. Patient past dental history revealed that she went extraction of one tooth in the upper left quadrant due to presence of dental decay. Patient was absolutely normal with no history of pain or pus discharge from the missing tooth region. On examination of her old dental reports, extraction of the maxillary left first molar followed by marsupialization of the cystic lesion involving the same tooth was apparent almost seven years back. On intraoral examination, clinical missing of maxillary left first molar was observed. For the replacement of missing tooth with single tooth implant-based prosthesis considering the patient’s young age, a cone-beam computed tomographic scan was advised. On CBCT scan, a well-defined radiolucency extending from maxillary left first molar tooth socket involving the entire left maxillary sinus was noticed [1-3]. Based on history, clinical features and CBCT scanning image reports, the case was provisionally diagnosed as residual cyst. Enucleation of entire cystic lesion under general anesthesia was performed and the specimen was sent for histopathological examination [4]. The histopathological evaluation report stated the presence of fibro-collagenous wall lined by stratified squamous epithelium and sub-epithelium with mixed chronic inflammatory cell infiltration. Based on histological report, finally the case was diagnosed as having radicular cyst involving left maxillary sinus (Figures 1-4).

DISCUSSION
A clinician or dentist may come across numerous odontogenic pathologic conditions like cysts and tumors during routine dental check-up. Recently, advanced imaging techniques like CBCT scan are of great helpful in diagnosing various pathologic conditions. A cyst may be defined as an epithelial lined pathologic cavity that may contain fluid or a semisolid material. Based on their origin, they can be classified as Odontogenic which arise from residues of enamel epithelium, and non-odontogenic cyst as they arise from lines of fusion and pseudocysts which arise from non-epithelial and lined only by connective tissue. These cysts are most common among other odontogenic cyst may be because of high incidence of pulpal pathology in the oral cavity [1,2]. There are reports showing the occurrence of inflammatory cysts following pulp therapy. Even the irritants present in the cements used during endodontic treatment will results in development of cysts in the future in children [12]. Nagaveni [13,14], published a case of lateral periodontal cyst and occurrence of eruption cysts in an Indian patient [13,14]. This shows the importance of awareness about occurrence of various cysts in children. In our case, past history of marsupialization of the cystic cavity shows the continued infection from the residual microbes must have led to spread of infection involving the maxillary sinus.
Regarding cysts occurring in the maxillary sinus, there are two types of cysts mentioned in the literature involving maxillary sinus. The first type is “intrinsic” type, when the cyst is derived within the antral wall or arise from the mucosa of the sinus, and the second type is “extrinsic” one, when it originates from Odontogenic source like maxillary tooth or may originate from adjacent vital structures like jaw bone. The intrinsic type includes retention cyst and mucoceles whereas extrinsic type consists of radicular cysts, keratocystic Odontogenic tumors, residual radicular cysts, calcifying cystic Odontogenic tumors and dentigerous cysts based on their prevalence in their occurrence. Among intrinsic type, mucous retention cysts are the most common type which typically characterized by originating from the floor or walls of the sinus. With regard to extrinsic type, the cysts are mostly of dental origin with dentigerous cyst arising from an impacted molar being most common. However, the final diagnosis of these varieties of maxillary cyst should be done only after their histological examination. Therefore, based on this classification, the case presented here was categorized as extrinsic type of cyst involving maxillary sinus and the final diagnosis of the same was confirmed following histological evaluation [5].
Most of the time, radicular cysts appearing in the maxillary sinus remain asymptomatic. This is because, the air-filled sinus and its thin walls provide less resistance to cystic growth, thus causing it to considerably increase in size before they become symptomatic and are clinically noticed by the patient [6]. The same clinical presentation of the radicular cyst was evident in our case. The cyst was diagnosed on CBCT scan which was done for the pre-implant prosthesis purpose. Other-wise patient was absolutely normal with no any facial swelling, dissymmetry pain or pus discharge in the oral cavity.
In differential diagnosis, other Odontogenic cysts which can involve the maxillary sinus should be considered such as nasopalatine duct cyst, odontogenic keratocyst and fissural cyst-like median palatal cyst. Clinically, the radicular cysts found to be associated with root apex of a carious tooth and they usually measure from a few millimeters to a centimeter in size [1.2]. However, there are few reports and including the present case showing large lesion of radicular cyst growing to engulf almost the entire maxillary sinus and hence, it is very essential to evaluate in detail when a common pathology shows an uncommon presentation to avoid misdiagnosis and to prevent unwanted post-surgical sequel.
On conventional radiographic examination, the radicular cyst appears as a unilocular radiolucent lesion with well-circumscribed radiopaque sclerotic borders. However, multi-locular presentation rarely encountered. The cyst is seen with the apex of the involved tooth root measuring with a diameter of more than 2 CMS in size. When the size of the lesion is large, it can engulf into the maxillary antrum, elevating its floor and causing it to appear as a thin plate of bone covering the lesion as seen in few case reports. This radiographic feature is helpful to classify the cyst as intrinsic or extrinsic type. However, for final diagnosis histological evaluation is essential to define it and to name the type of the cyst. In differential diagnosis, other odontogenic cysts need to evaluated as they present the same radiographic features such as Odontogenic keratocysts, dentigerous cysts, ameloblastoma, pindborg tumor, Odontogenic fibroma, cementomas and dentigerous cysts. In extensive cases, conventional 2-dimensional radiographic techniques like panoramic radiographs are not useful to elaborate the full extent of the lesions, and advanced imaging techniques are deemed useful [1-11].
Advanced 3-dimensional imaging techniques like CT scans and CBCT scans gives superior bony details, provides visualization of the size and extent of the lesion with determination of orbital or nasal invasion or involvement and extent of the lesion along with proximity to adjacent vital structures. In case of large cystic lesions, on CBCT or CT images, opacification of airspace within the maxillary sinus is observed. In addition to this, in case of larger lesions, this technique helps in planning of surgical treatments. It is even important for differential diagnosis of other Odontogenic cysts occurring in the maxillary sinus [6-10].
On histological examination, the histologic picture exhibits cystic lumen, lined by a thin epithelial lining containing microcellular connective tissue stroma, showing dense chronic inflammatory cell infiltrations with few cholesterol clefts [5-10]. It is a chronic inflammatory lesion characterized by having a closed pathologic cavity lined with either partially or completely non-keratinized stratified squamous epithelium. The underlying fibrous connective tissue wall is inflamed with varying degree of cell infiltration, which consists mainly of macrophages and small blood vessels. However, it is also reported that occasionally these cysts are found to be lined, partially or predominantly by columnar ciliated, epithelium or mucous secretory cells, which may be due to the migration of these cells from either the maxillary sinus or the nasal cavity, the metaplasia of the stratified squamous epithelium or to the differentiation of pluripotent cells within the jaw. In the present case reported here, the histopathological features were suggestive of radicular cyst.
The management of radicular cysts involving maxillary sinus differs in each case based on its size and extent of the lesion [4-10]. If the cyst is small, root canal treatment is suggested as it removes the microbes from the root canal, thereby reducing the invasion of microbes into the periapical region. Sometimes apicectomy is carried out if the infection is not resolved by endodontic therapy. If, both of these treatment options fail, then extraction of the offended tooth is done, followed by curettage of the periapical region. In case of larger sized cysts, surgical intervention including marsupialization and enucleation of the cyst is performed [1,2]. reported a case of radicular cyst in an 18-year-old male patient involving the maxillary sinus, which was treated by surgical intervention consisting of complete removal of the cyst and immediate reconstruction of the midfacial buttress using an autologous rib graft in a tongue-and-groove fashion [7]. described a rare case of radicular cyst associated with deciduous right upper molars in a 5 -year-old male patient. The cyst developed asymptomatically in the maxillary sinus, thereby causing considerable displacement of both premolar germs. Surgical enucleation of the cystic lesion carried out and the extent of the lesion, resulted in necessity of removal of the second premolar germ. They finally concluded from this report that early diagnosis of the lesion would have resulted in a more conservative treatment plan and emphasized on the endodontist’s role in early diagnosis of such lesions [8].
Although surgical intervention eliminates periapical pathology but to obtain bone regeneration and healing of periapical tissues, bone regeneration is essential to fill the bony defect. Autologous platelet-rich fibrin is an excellent healing biomaterial extensively used in oral surgical defects with the new perspective of accelerated healing due to presence of growth factors. Titanium-prepared platelet rich fibrin (T-PRF) is a third-generation platelet concentrate developed to overcome the harmful effects of silica in glass tubes and also has a longer resorption rate. Cevik [9] showed the effects of T-PRF applied to the bone defect that occurred after the enucleation of the radicular cyst in their case. A significant increase in bone density was observed after eight months of follow-up [9]. Consolo [10] performed a trans-nasal endoscopic marsupialization of voluminous radicular cyst involving the maxillary sinus and nasal cavity in their case.
- Shear M (1992) Radicular and residual cysts. Cysts of the oral regions. 3rd Wright: Oxfor, pp: 136-162.
- Bhaskar SN (1966) Periapical lesion, types, incidence and clinical features. Oral Surg Oral Med Oral Pathol 21: 65-72.
- Nilesh K, Dadhich A (2020) Unusual large radicular cyst presenting in the maxillary sinus. BMJ Case Rep 13: e236582.
- Anusha RL, Babu SG, Thomas PS, Castelino RL (2019) Radicular cyst involving maxillary sinus: A report of rare case. Int J Maxillofac Imag 5(1): 19-21.
- Amos MJ, Dalghous A, Alkhabuli J, Mizen KD (2007) Massive maxillary radicular cyst presenting as facial fracture and abscess. A case reports. Libyan J Med 2: 211-213.
- Bahadure R, Khubchandani M, Thosar NR (2013) Radicular cyst of primary tooth associated with maxillary sinus. BMJ Case Rep pp: 1-4.
- Hahn HM, Lee YJ, Park DH (2019) Huge Radicular Cyst of the Maxilla Treated with Complete Resection and Immediate Reconstruction by Rib Bone Graft. J Maxillofac Oral Surg 18(3): 378-381.
- Chybicki D, Lipczyńska-Lewandowska M, Ratajek-Gruda M, Janas-Naze A (2020) Massive Radicular Cyst in the Maxillary Sinus as a Result of Deciduous Molar Tooth Pulp Necrosis. Case Rep Dent 2020: 8837706.
- Cevik T, Genc FC, Koraltan M (2021) Management of maxillary radicular cyst by using the titanium-prepared platelet-rich fibrin (T-PRF): A case report. J Adv Oral Res 12(2): 310-313.
- Consolo U, Bellini P, Lizio G (2018) Trans-nasal endoscopic marsupialization of a voluminous radicular cyst involving maxillary sinus and nasal cavity: A case report and a literature review on this surgical approach. Oral Maxillofac Sur Cases 4: 91-96.
- Umashankara KV, Nagaveni NB, Manjunath S (2012) Ameloblastic fibro-dentinoma: Report of a rare tumor with literature review. J Cranio Max Dis 1: 141-144.
- Nagaveni NB, Umashankara KV, Radhika NB (2011) Inflammatory dentigerous cyst associated with an endodontically treated primary second molar. A case reports. Arc Orofac Sci 6(1): 1-5.
- Nagaveni NB (2023) Lateral periodontal cyst in a pediatric patient-Report of a rare case. J Pediat Dent Hyg 2: 7-8.
- Nagaveni NB, Umashankara KV, Radhika NB, Maj Satisha TS (2011) Eruption cysts: A literature review and four case reports. Ind J Dent Res 22: 148-151.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Allergy Research (ISSN:2642-326X)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Chemotherapy Research Journal (ISSN:2642-0236)